Candida is a fungus that normally inhabits the mouth, throat, gastrointestinal tract and vagina. Under normal conditions, candida exists within us in a healthy balance, and the body’s immune system keeps it from spreading. When your immune system is strong, candida yeasts presents no problem. However, poor and high sugar diets, nutritional deficiencies, exposure to toxins, stress and/or taking antibiotics or other medications could result in the good bacteria, that prevent fungal infections from developing, to be knocked out. Candida yeasts then multiply and further weaken the immune system.
What Is Candida Albicans?
Candida albicans is a species of yeast — a single-celled fungus, in fact – that lives naturally in the body. This yeast is a normal part of the microbes that live on your skin and in your gastrointestinal tract, but under some circumstances it can multiply out of control.
Small amounts of Candida albicans also live in various warm, moist areas throughout the body, including on the skin, in the mouth and gut, and also the rectum and vagina...Continue Reading (https://www.thecandidadiet.com/what-is-candida-albicans/  )
)
Symptoms of Candida
Feelings of frustration and loneliness are common when dealing with a yeast overgrowth because Candida is evasive to much of the medical community. Here are some of the common symptoms:
- Gas, bloating and indigestion
- Bowel irregularities, constipation or diarrhea
- Food cravings especially for carbohydrates or sweets
- Mood swings or depression
- Headaches or migraines
- Menstrual problems and PMS
- Dry, itchy skin or hives
- Finger or toe nail fungus
- Vaginal yeast infections
- Itching or redness in body creases
- Chronic fatigue and fibromyalgia
- Weight imbalances (over or under-weight despite diet)
- Premature aging
- Chemical sensitivity (especially colognes or fabric dye)
Dietary Changes in Reducing Candida
 Changing your diet is also recommend to control the Candida. Your diet should exclude fruit, sugar and yeast. Especially in the beginning of the treatment you have to be very strict and disciplined. If you cheat you’ll feel the effect of the Candida “monster”.
Changing your diet is also recommend to control the Candida. Your diet should exclude fruit, sugar and yeast. Especially in the beginning of the treatment you have to be very strict and disciplined. If you cheat you’ll feel the effect of the Candida “monster”.Anti-fungal agents can also be used. The major anti-fungal prescription medications are Nystatin, Diflucan, Nizoral and Sporanox. Natural antifungal and antibacterial agents are garlic, olive leaf extract, oil of oregano, pau d’arco, uva ursi, golden seal, caprylic acid and citrus seed extract. Fibers such as flaxseed powder and psyllium husk are also beneficial.
Balancing Act
Generally speaking, proper diet, high potency and quality multi-strain probiotics and natural anti-fungal agents are essential in the prevention, control and elimination of Candida.
As the intestinal and vaginal microflora become balanced, you can tolerate a greater variety of foods. If you think you might have symptoms of Candida overgrowth, consult a health care practitioner who is familiar with this condition. Other conditions have similar manifestations. Self-diagnosis and self-treatment may cause these conditions to be overlooked.
The main predisposing risk factors for fungal infection include alterations in immunity associated with broad-spectrum antibiotic therapy, poor and sugary diet, nutrient deficiencies, heightened toxic exposure, stress, underlying malignancy, HIV infection, organ transplantation, chemotherapy and other immunosuppressive drug therapy. These and other factors, such as changes in endocrine and metabolic balance, may enhance fungal colonization, alter the body’s inner ecology and lower host’s immune response.
C. albicans remains the most common infectious strain, accounting for approximately 50% of total Candida infections. Candida glabrata (8–18%), tropicalis (11–25%), parapsilosis (7–15%), and krusei (2–4%) have emerged as formidable players as well, and these pathogens display variable susceptibility to azole antifungal agents.
Candida species (spp) are a significant clinical problem for a variety of immunocompetent patients worldwide. Candidiasis has increased substantially in the past twenty years as Candida spp now ranks fourth among microbes most frequently isolated from blood cultures. They are also the most common opportunistic pathogen in AIDS patients. Paradoxically, modern medical practice which has prolonged the survival of a large number of patients, has also made them more susceptible to candidiasis(11).
The increased incidence of candidiasis, the increased resistance of Candida species to antifungal agents and the rise in lethality associated with infections by Candida spp has prompted renewed research on innovative ways to prevent and treat infections by these opportunistic yeasts. Medical advances are helping researchers understand the complexities of inner ecology including the interrelationship between Candida and various body systems. For example, vaginal candidiasis appears to coincide with C. albicans in the large intestine. When this occurs, successful treatment of intestinal overgrowth also addresses the health and balance of vaginal flora.
Candida and Probiotics
Probiotics provide Candida-inhibiting activities of commensal bacteria that reside in the alimentary and vaginal tracts of humans. Probiotic microbes not only suppress the growth of Candida spp in the alimentary tract and vagina, but they also inhibit the adherence of Candida spp to epithelial surfaces(11).
Lactobacilli and Bifidobacteria have the capacity to inhibit Candida spp. Each strain can have a different effect. That is the reason, Custom Probiotics formulates and supplies single and multistrain highest potency and quality probiotic bacteria for maximum effectiveness. We perform rigorous independent lab testing to verify the bacterial count of every batch to guarantee the potency of our probiotic dietary supplements.
A variety of mechanisms have been evoked to explain the anti-Candida activity of the probiotics. Nutritional competition, blocking receptors to Candida spp., adhesions on epithelial cells, production of anti-Candida compounds, increasing intestinal peristalsis, increasing intestinal epithelial cell renewal rates, alteration of pH and the production of an anaerobic oxidation-reduction potential (C. albicans is an aerobic microbe) have all been proposed as mechanisms that probiotic bacteria use to inhibit pathogens on mucosal surfaces.
The ability of probiotic bacteria to stimulate innate and acquired immune systems in the host and activate phagocytic cells is also thought to play a role in the inhibition of Candida spp. It is very likely that because of the recognized complexity of the aerobic and anaerobic normal flora, all the above factors are involved in the suppression of Candida spp. on mucosal surfaces. As a result, the inhibition of Candida spp. by probiotic bacteria, in the alimentary and vaginal tracts, represents a key, first-line defense against mucosal and systemic candidiasis.
All our Multi Strain Probiotics such as CP-1, D-Lactade Free Probiotics Powder, Six Strain probiotic powder and 11 Strain probiotic powder can be used for Candida.
 Factors that Promote Yeast Overgrowth
Factors that Promote Yeast Overgrowth
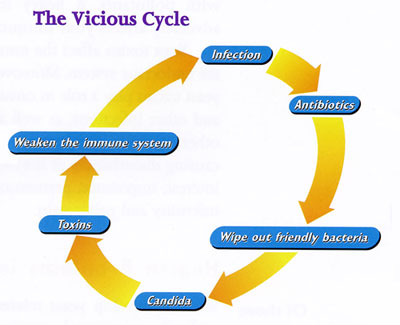
Like all fungi, Candida thrives in warm, moist areas. Under normal conditions, candida exists within us in a healthy balance, and the body’s immune system keeps it from spreading. If you take broad-spectrum antibiotics or other medications, good bacteria is compromised and candida yeasts are not affected. This results in the yeasts multiplying and releasing toxins that further weaken the immune system. Consequently, you may experience repeated infections, which may be treated with another round of antibiotics, encouraging further growth of candida ….and so the vicious cycle begins. (See diagram on the right).
Below is a list of factors that promote Candida overgrowth.
- Frequent or long-term use of antibiotics, such as tetracycline for acne
- Frequent use of broad-spectrum antibiotics for recurrent infections, such as in the ears, bladder, vagina, or throat
- Infections (digestive or otherwise) that lower the immune system, creating an imbalance in innate flora.
- Poor diet (junk and sugary foods)
- Stress or trauma
- Birth control pill use and hormone replacement therapy in women
- Painkillers
- Regular use of cortisone-type drugs
- Stimulants and depressants (caffeine, nicotine, alcohol)
- Diabetes (there will be more sugar in the blood and urine on which yeasts can feed)
- Pregnancy
- Eating disorders (starvation, vomiting, taking laxatives)
- Not being breast fed for the first six months
- Old age
- Vaccinations and immunizations
- HIV and AIDS
- Humid climates.
If you would like to know if your health problems are yeast-related, take the comprehensive Candida Questionnaire test taken from the book by W. G. Crook M.D., The Yeast Connection Click here to view or print out the questionnaire.
Candida Symptoms
Feelings of frustration and loneliness are common when dealing with a yeast overgrowth because Candida is evasive to much of the medical community. The following list of common symptoms are indicative of Candida overgrowth:
- Gas, bloating, indigestion, heartburn or pain in the intestines
- Bowel irregularities, constipation or diarrhea or perhaps alternating between the two
- Food cravings especially for carbohydrates or sweets.
- Mood swings, depression or suicidal tendencies
- Headaches or migraines
- Menstrual problems, PMS or break through bleeding, endometriosis.
- Respiratory concerns, asthma frequent bronchial congestion
- Dry, itchy skin or hives
- Finger or toe nail fungus
- Vertigo or balance problems
- Joint or muscle pain
- Bad breath despite good oral hygiene
- Allergies…air-born or food-related
- Malabsorption (might be indicated by vertical grooves in fingernails)
- Vaginal yeast infections
- Itching or redness in body creases
- Acne on face, back or body
- Cravings for chocolate, peanuts, pistachios or alcohol
- Adrenal or thyroid failure
- Hemorrhoids, fissure or rectal bleeding
- Insomnia
- Chronic fatigue
- Feeling cold and shaky
- Weight imbalances (over or under-weight despite diet)
- Poor memory
- Puffy, dry or burning eyes
- Urinary tract problems (infections, prostatitis, incontinence)
- Premature ageing
- Chemical sensitivity (especially colognes or fabric dye)
- Blood sugar imbalances
- Thrush/Gum Receding
- Numbness
Candida Mode of Action
When candida species proliferate beyond their normal numbers, the trouble starts. Increased levels of candida often initiate the proliferation of long root-like structures (mycelia and rhizoids) that penetrate the mucosal membranes, creating microscopic breaks in the normal mucosal boundary of the gastrointestinal tract. The resulting perforations permit antigens — foreign substances such as candida and its toxic acetaldehyde byproducts, other toxins, and incompletely digested dietary proteins — to leak into the bloodstream, which in turn creates antibody release and inflammation.
The Leaky Gut Connection
Microecology of the gastrointestinal tract can be divided into four major components (Fig. 3):
- the epithelial lining and mucosa of the gut wall the specific functions of which vary throughout the intestinal tract;
- the gastrointestinal secretions that enter the hollow organ;
- the intestinal microflora that live within the gut; and
- foods that are fed into the tract.
Figure 3. Components of the gastrointestinal ecology are depicted.
The epithelium of the small bowel is essential for the absorption of all major nutrients. Fermentation in the colon of dietary fibers leads to the production of a number of end products, including gases such as hydrogen, methane and carbon dioxide, as well as short-chain fatty acids (SCFAs). The predominant SCFAs are acetate, propionate and butyrate. SCFAs are almost entirely absorbed by the colonic mucosa and thus provide a source of energy to the host. The integrity of the epithelium of the esophagus, stomach as well as small and large bowels is essential in maintaining the balance of the microecology.
The lactic acid and the SCFAås mainly acetate, propionate and butyrate are predominantly produced in the first part of the large intestine (the ascending or proximal colon, fig. 4), while the phenolic and the nitrogenous compounds are produced in the descending (distal) and the sigmoid colon where many gastro-intestinal disorders develop.
Intestinal permeability, called “leaky gut” syndrome, is a common but poorly recognized problem linked to ecological disturbances. Individuals with leaky gut syndrome experience a wide range of problems including allergic responses, mood swings, depression, agitation, joint and connective-tissue pain and inflammation, headaches, irritable bowel syndrome (IBS), fatigue, and skin problems. Long-term “leakiness” may also predispose an individual to autoimmune responses such as Crohn’s disease (inflammatory bowel disease) and rheumatoid arthritis.
Leaky gut syndrome is linked to factors that predispose a person to intestinal microflora imbalances and irritation of the gut wall lining. Eliminating candida requires addressing the body’s ecological balance, its gut integrity and overall immunity.
How Can Someone Tell They Have Candida?
Candida symptoms are many, as indicated earlier.
You can identify candida overgrowth and monitor your treatment by having your doctor order some simple lab tests. Common diagnostic tests to determine the presence of candida and leaky gut include the following:
- Candida Immune Complexes is a blood test that has been proven to be effective in the detection and monitoring of candida overgrowth (Candidiasis). Candida Immune Complexes correlate to clinical symptoms of Candidiasis;
- Candida antibody panel (IgG, IgM, IgA) ( is a blood test);
- Intestinal permeability testing for leaky gut syndrome (a blood test); and
- Digestive stool analysis and culture.
These tests help health care practitioners detect candida overgrowth, measure your resistance levels and determine your digestive efficiency and the presence of leaky gut. Food allergy screening (including IgG), which exposes delayed or hidden food responses, gluten sensitivity screening, and immune profiles further refine the therapeutic program.
How Can Candida Be Controlled?
Candida is very complex and creates havoc in the intestinal and vaginal flora. Sometimes the best way to combat it is by outsmarting it. The more imbalance that exists the greater the symptoms (as indicated above).
Three proven strategies can be used to control or get rid of candida, as depicted in the diagram below:
1. Diet and Fiber
Nutritional programs including internal cleansing are one approach to controlling candida overgrowth. As indicated above, diet should exclude fruit, sugar and yeast. Especially in the beginning of the treatment you have to be very strict and disciplined. You will find out about the importance of diet, when you “cheat” and feel the effect. You have to be tuned to your body and understand why symptoms come and go. Without that understanding, it will be difficult to control the Candida “monster”. That is the reason we have included a lot of information on our website regarding this and other issues related to microflora balancing.
The following dietary suggestions are important to follow:
1. Eliminate or minimize the use of antibiotics, steroids, immune-suppressing drugs and oral contraceptives (only after consulting with your health care provider or physician).
2. Change your diet to one that will not encourage the growth of Candida. Eliminate fruit and fruit juices, sugar and other sweeteners including honey, cheese, dairy products and yeast. Candida thrives in a sugary environment, so your diet should be low in carbohydrates and contain no yeast products or sugar in any form. Soy sauce, mushroom, breads with yeast, baked goods and peanuts should be eliminated, as should any refined foods and any foods to which you are allergic or sensitive. Avoid coffee, soda and alcoholic beverages, as well as any fermented foods or beverages such as vinegar.
3. Eat plenty of vegetables and lean protein. The following foods are beneficial: most vegetables, especially broccoli, kale, garlic, turnip greens, onions, cabbage, eggs, fish and chicken. Homemade soups and stews are excellent. Substitute yeast-free millet bread with gluten free grains such as millet and quinoa. Limit potatoes, beets, carrots and corn.
4. Drink plenty of distilled or purified water: about 6-8 glasses a day.
5. Enhance digestion by eating more raw foods, chewing thoroughly and taking enzymes with every meal.
6. By re-establishing beneficial flora in your intestinal tract with acidophilus and bifidus supplements, you can help restore the normal balance of flora in the bowel and vagina. Our custom blend probiotics, including the Adult Formula CP-1 are available in multiple strains to address various issues. Candida or other pathogenic bacteria, for example, cause higher intestinal flora imbalance. In this case, a higher dosage of multistrain probiotic culture is recommended to overcome the resistance created by these pathogens. Dosage differs from person to person varying from 50 billion cfu’s per day to 500 billion or even more. Gradual dosage increase will help determine the optimum dosage for each individual. In addition to taking probiotics, increasing fiber consumption will also assist in absorbing and removing toxins from Candida die off. Staying on probiotic supplements while maintaining a healthy high fiber diet, will allow you to slowly reintroduce fruits and grains to your regimen.
7. Improve immune function by stimulating lymph flow through exercise and deep breathing.
8. Increase fiber consumption. This will help absorb and sweep out the toxins that are being created as Candida dies off. Ground flaxseeds are an excellent source of soluble and insoluble fiber, rich in omega-3 fatty acids, antioxidants, and phytochemicals called lignans. Colloidal bentonite and psyllium husk are also effective fibers.
9. Cleanse your system with herbs that help reduce Candida.
10. Repairing the intestinal wall and healing the ‘leaky gut’ by replacing or augmenting nutrients that support gastrointestinal mucosal healing. Vitamins, minerals, L-glutamine and fiber work synergistically to heal the intestines. A program including glutathione, N-acetylcysteine, milk thistle, dandelion, B-complex vitamins and a range of antioxidants can further help the liver in the detoxification process.
11. Stay on a probiotic and fiber supplement and continue on a maintenance diet and add back fruits and grains slowly!!
12. Probiotic retention enemas performed once a week or month, to replace “friendly” intestinal bacteria is also beneficial. Candida reside mainly in the colon and especially in the lowest part of the colon. This is due to a progressive increase in bacterial numbers and diversity towards more distal regions of the colon, where many gastro-intestinal disorders can develop (see fig. 5 bellow and table 1 in the section “What Are Probiotics?”). Also, the usage of anti-Candida medications may accumulate part of the “dead” Candida in the descending and sigmoid colon and hence their removal is beneficial.
Since the majority of “friendly” bacteria in the colon are bifidobacteria and some lactobacilli, a mixture of pure probiotic powder, dissolved in water and injected as an enema can be helpful to replenish the flora in the lowest part of the colon.
2. Probiotics: Custom Probiotics Adult Formula CP-1 and Six-Strain Formulation
As indicated earlier, causes of Candida are manifold including changing of the intestinal and vaginal microflora, which create an imbalance between good and bad bacteria. The more imbalance that exists, the more symptoms are varied. In addition, the strain type of candida overgrowth affects the severity of symptoms and duration of treatment.
Please note dosage differs from person to person. PLEASE CLICK HERE FOR COMPLETE DOSAGE SUGGESTIONS.
3. Anti-Fungals
The major anti-fungal prescription medications are: Nystatin, Diflucan, Nizoral and Sporanox. Natural antifungal and antibacterial agents are garlic, olive leaf extract, oil of oregano, pau d’arco, uva ursi, golden seal, caprylic acid and citrus seed extract.
Generally speaking, proper diet, high potency and quality multi-strain probiotics and natural anti-fungal agents should be first priority in the prevention, control and elimination of Candida. If you have a more virulent Candida strain, you may require prescription medication. The kinds and dosages of prescription anti-fungals should be determined by your health care provider, based on your stool, urine and/or blood analyses. Simultaneously, the use of highest potency and quality multi-strain probiotics is essential.
As the intestinal and vaginal microflora become balanced, you can tolerate a greater variety of foods.
Other conditions have similar manifestations. Self-diagnosis and self-treatment may cause these conditions to be overlooked. If you think you might have symptoms of candida overgrowth, we recommend that you first consult with a health care practitioner familiar with this condition then speak to us about which custom blend probiotic is right for you.

